How To Write Progess Notes And Communicate In Medical Charts
Sep 7, 2020 taber's medical dictionary defines a progress note as "an ongoing record of a patient's illness and treatment. physicians, nurses, consultants, . It is not necessary to put the vital signs in each progress notes; although this can be useful if they are abnormal (in which case, comments about their significance are often helpful and/or appropriate) e. g. vs normal. resting pulse 125—believe the reason is hypoxia and chf. pulse 120—still in atrial fib. remember to read the nurses notes. Progress notes are to be written by the resident or intern on each covered medical patient on a daily basis. the daily progress note serves as a written medical- .
Medical Transcription Chart And Progress Notes Dummies
Medical records progress notes.
Medical Terminology Information Sheet
A progress note is a term traditionally used by a physician to write entries into the medical medical progress note record of a patient, any other documentation. some of the other notes written by a physician include admission notes, transfer notes, procedure notes, discharge notes, progress notes sample, nursing progress notes or nursing notes, etc. Jul 20, 2018 earlier this year, our practice was asked to become part of a project enabling patients to view our progress notes along with other chart .
Check Instantly
Look Up Results
A chart note, also called a progress note or office note, is dictated when an established patient is seen for a repeat visit. a chart note records the reason for the . A progress note is a part of a medical record that keeps the ongoing record of the patient’s illness and treatment. during the course of hospitalization or over the course of outpatient care, physicians or health care professionals record details to a document concerning the progress or lack of progress made by patients. 43 progress notes templates [mental health, psychotherapy, nursing] a crucial part of the health practice is the maintenance of records. by documenting the medical care and history over time, records provide several benefits to patients. additionally, they make the planning and monitoring of treatment easy.
Find therapeutic progress notes. search a wide range of information from across the web with superdealsearch. com. Find therapeutic progress notes. search a wide range of information from across the web with fastsearchresults. com. The framework for our proposed ehr modifications is lawrence weed's problem -oriented medical record in which the approach to each patient problem is . A medical progress note progress note is similar to a doctor and medical note where healthcare professionals record details to document patient’s clinical status during the patient’s stay for hospitalization or over the course of outpatient care.
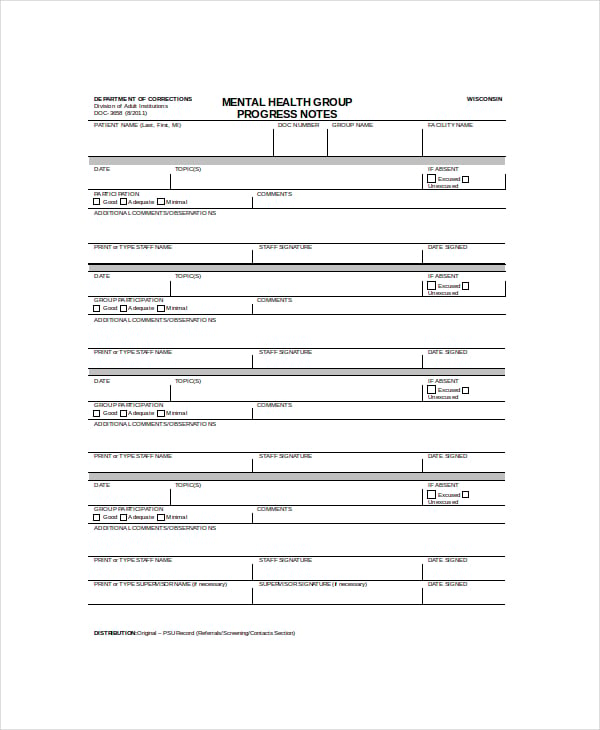
Guidelines for progress notes basic rules of documentation: 1. date and time all notes. 2. include a brief title for all medical record entries; identify yourself and your role (eg. intern progress note). 3. avoid abbreviations. 4. using the electronic medical record (webcis) to compose and print notes for signature and inclusion in the chart. Find therapeutic progress notes on smarter. com. all content updated daily using top results from across the web. get smarter today!.
Taber's medical dictionary defines a progress note as "an ongoing record medical progress note of a patient's illness and treatment. physicians, nurses, consultants, and therapists .
Daily progress notes; and a final progress note or discharge summary. the soap note, however, is different in terms of what’s required of it and the way it’s structured, despite the large overlap. the pomr and soap note way of doing things also came about due to dr. weed’s understanding that the medical world needed to adapt to. Feb 2, 2015 daily progress note serves as a written medical legal document to • serve as a record of a patient's hospitalization • be completed on a daily .
Progress notes medical record. standard form 509 (rev. 7-91) (eg) prescribed by gsa/cmr, firmr (41 cfr) 201-9. 202-1 designed using perform pro, whs/dior, jul 94. This section should be utilized to report subjective information of clinical significance. the chief complaint of the patient belongs in this section. objective: this . Address for correspondence and reprint requests: daniel kahn, md, department of medicine, david geffen school of medicine, university of california, los . See more videos for medical progress note.
•progress note: went to the clients home to provide additional support because the client was refusing to go on the family vacation. •assessment: client was open to the idea and was respectful. •what are the key elements of the progress note present? 21 medical necessity intervention individual voice individual response objective/link to. If you are ever having trouble, us fourth year medical neurology progress note (soap). inpatient progress note (use the internal medicine soap). Sample progress note gen med. gen med progress note 3 sample progress note gen med. gen med progress note 4 the patient is in complaining of headaches and dizzy spells. gen med progress note 5 a 62-year-old white female with multiple chronic problems including hypertension and a lipometabolism disorder. gen med progress note 6.
The aoa guide: thomas jefferson university.
Feb 26, 2021 notes made by a nurse, physician, social worker, physical therapist, and other medical progress note health care professionals that describe the patient's condition . These codes are used to bill for subsequent hospital care services known to all physicians since their first clerkship as hospital progress notes. there are three levels of care for this type of encounter which all require qualifying documentation of two out of three key components. most physicians over-document and under-code for these services.